Long-Term Follow-up of Congenital Hypothyroidism with Delayed Diagnosis
Dr. Gita Sharifi
Medical Lab, licensed by Shahid Beheshti University of Medical Sciences, Department of Clinical Laboratory Sciences. Tehran/Iran
APFCB News Volume 4, Issue 2, 2025
Introduction
Congenital hypothyroidism (CH) is one of the most common endocrine disorders in neonates. As thyroid hormones are so important for brain growth, neonatal screening allows early detection and treatment, but missed cases can result in delayed therapy. Symptoms such as excessive sleep, calmness, and prolonged constipation may suggest hypothyroidism but are often underestimated. This case shows a patient with missed screening and long-term follow-up up to adulthood.
Case Presentation
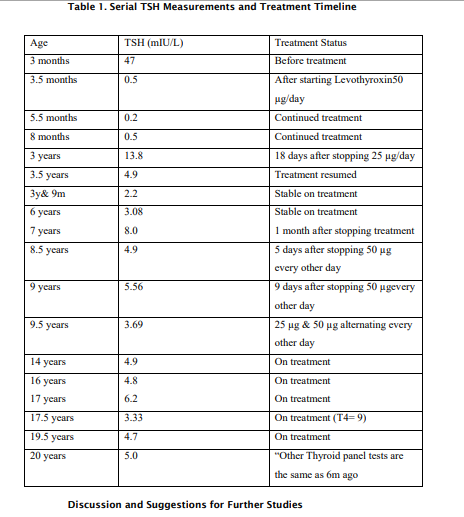
A female infant was not screened for CH several days after birth. She was a full-term newborn weighing 3 kg at birth. Her mother noticed excessive calmness and sleeping throughout the night, and sometimes long periods of sleeping in the evenings. At 2.5 months, after 20 days of no bowel movements and constipation, she was referred to a pediatrician. Following rectal touch, she had a large amount of stool excretion, and after that, thyroid testing showed TSH = 47 mIU/L. A pediatric endocrinologist started Levothyroxine 50 µg/day at age 3 months, and TSH dropped to 4.5 mIU/L soon after. At age 3, thyroid ultrasound confirmed normal size and location. When therapy was stopped for 18 days, TSH rose to 13.8 mIU/L (Table 1)
She was followed up regularly. TSH remained normal under consistent Levothyroxine therapy. At7 years, another endocrinologist recommended discontinuing Levothyroxine for 1 month. TSH increased to 8 mIU/L, but despite that, therapy was initially stopped. Later, other endocrinologists advised continuation, one of them believed to keep TSH under 5, and therapy resumed. From age 10, she was under pediatric endocrinologist visits every 4–6 months. For height growth delay, she received Diphereline (GnRH agonist) monthly and Nordilet (growth hormone) daily. At age 14, after achieving physiological puberty, GH therapy was stopped. Levothyroxine continued until age 18,and the thyroid status was under control. After that the therapy was stopped for 1 year, causing TSH to rise to 5.5 to 6 mIU/L. Then at the age of 20 the endocrinologist asked her to take Levothyroxine 220 ug/week, resulting in stable TSH between 3–4 mIU/L, but each time she was stopping treatment, TSH would rise to 4.8 to 5.2mIU/L, and she experienced some hair loss, hypersomnia, and occasional constipation, indicating subclinical hypothyroidism after discontinuation of Levothyroxine. The test results with ECL method at the age of 20 were as below:
TSH= 3.33 mIU/L, FT4= 1.42 ng/dL, Total T4= 8.62 ug/dL, T3= 86.8ng/dL, FT3= 3.9pmol/L Endocrinologists now suggest that TSH levels below 10 mIU/L do not always require treatment, but FT4 must be considered. So now at the age of 22 she has stopped the treatment for 2 years, and the test results are as follows: TSH(ECL)=5.64mIU/L, FT4(ECL)=1.17 ng/dL (RR=0.7-1.8), Total T4=7.36 μg/dL.
Table 1. Serial TSH Measurements and Treatment Timeline
Discussion and Suggestions for Further Studies
It was a retrospective study on a case of congenital hypothyroidism from birth through adolescence. The diagnosis was delayed and confirmed at 2.5 months of age, and Levothyroxine therapy was initiated thereafter at the age of 3 months and continued until the age of 20 years. After discontinuation of Levothyroxine, TSH stabilized around 5 mIU/L. After that, it was asked about whether this condition still qualifies as subclinical hypothyroidism and whether continued treatment is necessary, and whether there are some problems left.
There are some guidelines in AAP(American Academy of Pediatrics) or ESEP(European Society for Pediatric Endocrinology) about the appropriate time for screening and diagnosis after birth (for example CH screening is necessary for all newborns up to 48 to 72 hours after birth and before hospital discharge), treatment and its follow-up and discontinuation of treatment (for example, short-term discontinuation at the age of 3 years and recheck the TSH and FT4 after 1 month) to check whether it is transient or temporary CH and the definition of the term subclinical hypothyroidism. (1-3) Necessary to say that in this case, after rising TSH>10 mIU/L following discontinuation of treatment at the age of 3 years, the endocrinologist strictly didn’t allow stopping the medication again until around the age of 7 years due to its adverse effects on brain development.
There are some articles and their links related to this subject that refers to AAP and ESEP
guidelines. (4-6)
Suggestions for further studies:
Future studies should investigate the impact of early iodine exposure, such as Betadine use, in neonates with a genetic predisposition to hypothyroidism. It is also recommended to assess the long-term outcomes of patients with congenital hypothyroidism (CH) who discontinue treatment despite having TSH levels above 5 mIU/L. Further research should explore whether clinical symptoms like hair loss, hypersomnia, and constipation justify restarting therapy in patients with TSH levels between 5 and 10 mIU/L. Additionally, surveying adults with undiagnosed CH who present with mild thyroid dysfunction could provide insights into the relationship between delayed treatment during childhood and their psychosocial development. Finally, studies should examine any association between CH and delays in physical growth rate, particularly around puberty or earlier stages of growth.
Conclusion
CH can be a temporary position, and severity may decrease after birth, and shortly delayed diagnosis may be managed successfully, especially if the thyroid gland is normal in size and structure, and position, and therapy is maintained soon after. This patient showed normal intellectual, emotional, and social development. In this case, a 3-month delay in starting treatment had no negative impact on IQ or developmental outcomes. Symptoms like hypersomnia and hair loss reappeared upon discontinuation at the age of 22 years, indicating persistent subclinical hypothyroidism, but now some endocrinologists believe that TSH around 5 mIU/L is normal and these symptoms are not related to thyroid status, and even with TSH up to 10 mIU/L but FT4 within the Reference range, there is no need for treatment.
Authors Contribution:
All authors are independent experts and equally contributed to the
expert article published. Funding: None declared
Conflict of Interest: None declared
1. Léger, J., Olivieri, A., Donaldson, M., Torresani, T., Krude, H., Van Vliet, G et al. European Society for Paediatric Endocrinology consensus guidelines on screening, diagnosis, and management of congenital hypothyroidism. The Journal of Clinical Endocrinology & Metabolism, 99(2), pp.363-384. 2014;81(2):80-103.
2. Van Vliet G, Grosse SD. Newborn screening for congenital hypothyroidism and congenital adrenal hyperplasia: the balance of benefits and costs of a public health success. Medecine sciences: M/S. 2021 May 18;37(5):528
3. Kapelari K, Kirchlechner C, Högler W, Schweitzer K, Virgolini I, Moncayo R. Pediatric reference intervals for thyroid hormone levels from birth to adulthood: a retrospective study. BMC endocrine disorders. 2008 Nov 27;8(1):15.. 4. Rose SR, Wassner AJ, Wintergerst KA, Yayah-Jones NH, Hopkin RJ, Chuang J et al. Congenital hypothyroidism: screening and management. Pediatrics. 2023 Jan 1;151(1).
5. Behura SS, Nikhila GP, Panda SK. Screening and management of congenital hypothyroidism—Guidelines by American academy of pediatrics, 2023. Indian Pediatrics. 2023 Oct;60(10):855-8.
6. Grob F, Lain S, Olivieri A. Newborn screening for primary congenital hypothyroidism: past, present and future. European Thyroid Journal. 2025 Apr 1;14(2)