Unveiling the clinical conundrum: coexistence of Gilbert’s syndrome and Thrombocytopenia
Dr. Cheteny Cheteny, Dr. Enitarast Sympli, Dr. Kapil Kumar, Dr. Chillarige Sudha Ankita, Dr. Swati Singh
1,2,4,5Department of Biochemistry, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, New Delhi, India
3Department of Gastroenterology, Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, New Delhi, India
APFCB News Volume 4, Issue 2, 2025
INTRODUCTION
Gilbert’s syndrome (GS) is an autosomal recessive disorder caused by a defect in bilirubin conjugation, due to mutations in in the promoter region of the Uridine Glucuronosyltransferase 1A1 (UGT1A1) gene, resulting in diminished UGT1A1 enzyme activity. This enzyme typically conjugates bilirubin, facilitating its clearance from the bloodstream [1]. It has about ~20% prevalence among the Indian population [2]. The global incidence of GS is about 5%, more common in males, often manifesting as mild jaundice, without liver dysfunction, but some patients have abdominal discomfort, fatigue, nausea, etc., which may be caused by anxiety and other psychological factors. Albeit 33% of individuals remain undiagnosed due to the asymptomatic nature of the condition [3,4].
Literature suggests that GS is associated with a mild unconjugated hyperbilirubinemia, increased circulating antioxidant capacity, and reduced cardiovascular disease (CVD) risk [5]. Prior studies have substantiated that circulating unconjugated bilirubin (UCB) is negatively associated with multiple thrombotic risk factors including platelet activity, hemostatic function, and inflammation in individuals with GS [6-9]. Here, we present a rare case of a 40-year-old man found to have Gilbert’s syndrome, who presented with moderate thrombocytopenia, with no known trigger or coexisting condition. It is important to clarify the cause of thrombocytopenia in individuals with GS, as such cases are often clinically misdiagnosed as hemolytic jaundice, and may lead to repeated liver tissue biopsies, thereby causing psychological and economic strain on individuals with GS.
CASE REPORT
A 40-year-old male laboratory staff presented for the voluntary routine health check-up at Govind Ballabh Pant Hospital, New Delhi, in June 2025, where laboratory investigations revealed elevated levels of unconjugated bilirubin. On detailed questioning, he reported that he had no complaints of jaundice, fatigue, bleeding, bruising, abdominal pain, pale stools, dark urine or any constitutional symptoms and also had no history of alcohol consumption and chronic drug intake. His past medical history was positive for thrombocytopenia.
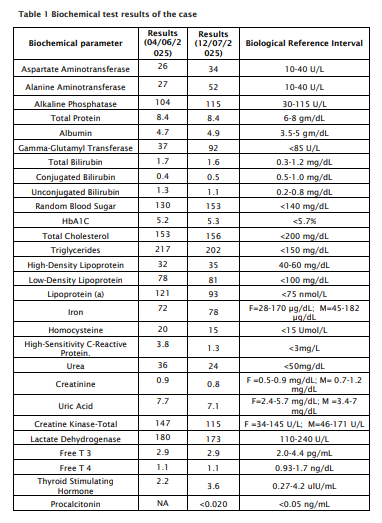
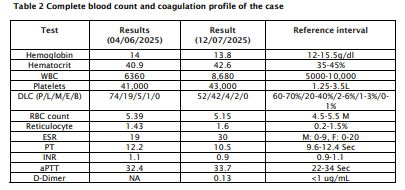
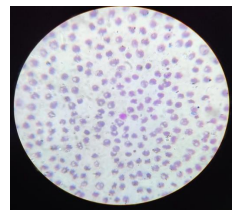
On examination, he was noted to be in apparently healthy state, with a robust build and stable vital signs. Abdominal findings were otherwise unremarkable and there were no stigmata of chronic liver disease on systemic evaluation. Laboratory results revealed a hemoglobin of 13.8 g/dL, MCV of 87 fL and a normal white blood cell count, while platelet count was low at 43,000/µL. No hemolysis was evident on peripheral smear: His direct bilirubin, LDH and liver function tests were all within normal limits (Table 1 and 2). Viral hepatitis serologies (HBsAg and anti-HCV) were negative, and abdominal ultrasound did not indicate abnormal liver morphology. Fibroscan showed no signs of liver fibrosis and the liver elasticity was within normal limits. ANA, dsDNA and RA factor were performed to rule out autoimmune causes for hemolysis and were found to be within normal limits.
The diagnosis was made on the basis of a mild unconjugated hyperbilirubinemia in the presence of repeated normal liver function tests and absence of overt signs of hemolysis on clinical presentation.
WBC: White Blood Cell; DLC: Differential Leukocyte Count; P: Polymorphonuclear leukocytes; L: Lymphocytes; M: Monocytes; E: Eosinophils; B: Basophils; ESR: Erythrocyte Sedimentation Rate; PT: Activated Partial Thromboplastin Time; INR:International Normalized Ratio; aPTT:Activated Partial Thromboplastin Time; NA: Not available
Figure 1 Peripheral blood film of the case showing normocytic normochromic RBCs with reduced platelet count 50,000/µL. Wright-Giemsa stain, magnification ×100
DISCUSSION
The incidence of a thrombocytopenia in Gilbert’s syndrome is rare. What renders our case particularly unique is the markedly reduced platelet count (43,000/µL) in the absence of any overt clinical manifestations. This value is lower than any previously documented case in the existing literature. Several publications were reviewed in an attempt to identify potential pathophysiological mechanisms underlying comparable observations within the GS population.
In a previous investigation by Sarlak et al. involving 1,082 individuals with GS and 1,084 healthy controls, the researchers documented significantly reduced platelet counts among GS cohort (240300/µL) compared to control group (258000/µL) (p<0.001). Additionally, they identified an inverse association between UCB levels and neutrophil-to-lymphocyte ratio and platelet-tolymphocyte ratio. The authors proposed that UCB confers cardioprotective effects by exerting antioxidative and anti-inflammatory mechanisms [6]. In line, a recently published study involving 68 individuals with GS and 68 healthy controls demonstrated that mean platelet volume (P < 0.001) was significantly reduced in the patient group compared to the controls [7]. Kumar N et al. observed that elevated UCB contributes to thrombocytopenia via mitochondrial ROS-driven
antioxidative and anti-inflammatory mechanisms [6]. In line, a recently published study involving 68 individuals with GS and 68 healthy controls demonstrated that mean platelet volume (P < 0.001) was significantly reduced in the patient group compared to the controls [7]. Kumar N et al. observed that elevated UCB contributes to thrombocytopenia via mitochondrial ROS-driven activation of p38 and p53 pathways. They found that UCB induced platelet apoptosis, marked by increased ROS, mitochondrial depolarization, calcium influx and cardiolipin peroxidation [8]. In an earlier in-vitro investigation, Suvansri U et al demonstrated that exposure of platelets to UCB induced morphological alterations such as swelling, filamentous membrane formation and lysis. Additionally, pretreatment with UCB impaired thromboplastin generation, and inhibited clot retraction. The authors suggested that these abnormalities in platelet function were related to an inhibitory effect of bilirubin on ATP-ADP-dependent systems [9]. Similarly, Kundur et al. and Tapan et al. reported reduced soluble P-selectin levels in GS, which may decrease thrombus risk by limiting stable platelet-leukocyte aggregate formation [10,11]. Taken together, these findings suggest that UCB confers anti-thrombotic and cardio-protective effects by exerting anti-oxidative and anti-inflammatory mechanisms.
Several case reports have described an association between GS and reduced oxidative stress induced platelet hyper-reactivity. Haixia L and Li R discussed a case involving a primigravida identified having gestational diabetes mellitus with GS. Bilirubin has been negatively associated with type 2 diabetes, likely due to its lipid-lowering and antioxidant effects. Authors posited inhibition of NAD(P)H oxidase activity may reduce superoxide production in diabetic vascular tissue, thereby mitigating oxidative stress and preventing vascular complications [12]. Bilirubin's ability to attenuate various pathways that promote platelet hyper-reactivity and thrombus formation has, to date, been largely underappreciated in the literature. To our knowledge, the current report is the first documented case report to specifically detail thrombocytopenia in association with Gilbert’s syndrome.
CONCLUSION
In this paper, we reported a case of Gilbert’s syndrome with moderate thrombocytopenia, which is a rare ?clinical finding. Our case did not have the severe symptoms or outcomes as other reported patients. This study underscores the need for a comprehensive approach when managing patients with unexplained thrombocytopenia, where genetic disorders should be considered in the differential diagnosis. It also highlights the diagnostic complexity and the importance of laboratory findings, which is crucial for avoiding misdiagnosis in GS.
ACKNOWLEDGMENT
The authors acknowledge the support and assistance provided by the laboratory staff of the Department of Biochemistry, GIPMER
AUTHOR CONTRIBUTIONS
Cheteny C identified the patient case, coordinated with the patient and completed the diagnostic workup and prepared the initial draft of the manuscript. Sympli E assisted in taking a detailed clinical history, was responsible for blood sample withdrawal and collection of biochemical test reports. Kumar K aided in the clinical diagnosis and provided valuable clinical insights. Ankita CS conceived the idea, helped in writing and provided intellectual content, contributed in extended clinical workup and investigations. Singh S supervised the entire study, contributed in writing and critical review of the manuscript. All authors reviewed and approved the final manuscript.
CONSENT
The patient provided his written informed consent to participate in this study and for the publication of any potentially identifiable images or data included in this article in accordance with the 1964 Helsinki declaration and its later amendments.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
1. De Silva AP, Nuwanshika N, Niriella MA, de Silva HJ. Gilbert's syndrome: The good, the bad and the ugly. World J Hepatol. 2025 Feb 27;17(2):98503. doi: 10.4254/wjh. v17.i2.98503. PMID: 40027563.
2. Black M, Billing BH. Hepatic bilirubin udp-glucuronyl transferase activity in liver disease and gilbert's syndrome. N Engl J Med. 1969 Jun 5;280(23):1266-71. doi: 10.1056/NEJM196906052802303. PMID: 5770050.
3. Sticova E, Jirsa M. New insights in bilirubin metabolism and their clinical implications. World J Gastroenterol. 2013 Oct 14;19(38):6398-407. doi: 10.3748/wjg. v19.i38.6398. PMID: 24151358
4. mellie WS, Ryder SD. Biochemical "liver function tests". BMJ. 2006 Sep 2;333(7566):481-3. doi: 10.1136/bmj.333.7566.481. PMID: 16946336
5. Vítek L, Jirsa M, Brodanová M, Kalab M, Marecek Z, Danzig V, Novotný L, Kotal P. Gilbert syndrome and ischemic heart disease: a protective effect of elevated bilirubin levels. Atherosclerosis. 2002 Feb;160(2):449-56. doi: 10.1016/s0021-9150(01)00601-3. PMID: 11849670.
6. Sarlak H, Arslan E, Cakar M, Tanriseven M, Ozenc S, Akhan M, Bulucu F. Relation between unconjugated bilirubin and RDW, neutrophil to lymphocyte ratio, platelet to lymphocyte ratio in Gilbert's syndrome. Springerplus. 2016 Aug 22;5(1):1392. doi: 10.1186/s40064-016-3085-5. PMID: 27610311
7. Cure MC, Cure E, Kirbas A, Cicek AC, Yuce S. The effects of Gilbert's syndrome on the mean platelet volume and other hematological parameters. Blood Coagul Fibrinolysis. 2013 Jul;24(5):484-8. doi: 10.1097/MBC.0b013e32835e4230. PMID: 23348429.